AN EVIDENCE-BASED GUIDELINE FROM THE INTERNATIONAL COMMISSION FOR MOUNTAIN EMERGENCY MEDICINE (ICAR MEDCOM)
From vol. 103, spring 2013
By Jeff Boyd (a,b), Hermann Brugger (b,c), Fidel Elsensohn (b), and Peter Paal (b,d)
a) Department of Emergency Medicine, Mineral Springs Hospital, Banff, AB, Canada; International Federation of Mountain Guides
b) International Commission for Mountain Emergency Medicine ICAR MEDCOM
c) Institute of Mountain Emergency Medicine, EURAC Research, Drususallee 1, I-39100 Bozen/Bolzano, Italy
d) Department of Anaesthesiology and Critical Care Medicine, Innsbruck Medical University, Anichstrasse 35, A-6020 Innsbruck, Austria

AIRWAY PATENCY. IN BURIALS LONGER THAN 35 MINUTES, THE PATENCY OF A VICTIM'S AIRWAY BECOMES A CRITICAL OBSERVATION. IF THE AIRWAY IS PATENT THE VICTIM MAY SURVIVE, EVEN IF THEY ARE IN CARDIAC ARREST DUE TO HYPOTHERMIA. // HERMANN BRUGGER ARCHIVES
BACKGROUND
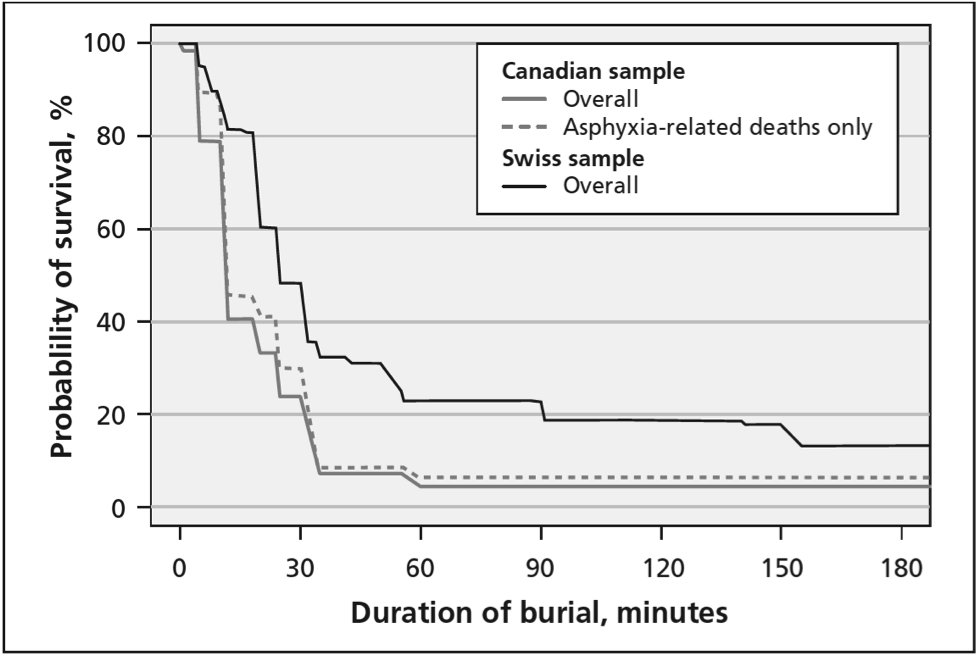
Medical management recommendations (Brugger et al., 2004; Brugger and ICAR1, 2006) have been previously based on concepts extrapolated from the avalanche survival curve derived from biostatistical analysis (Falk et al., 1994). A recent study comparing Canadian to Swiss survival produced similar sigmoidal-shaped curves (Fig. 1)(Haegeli et al. 2011).
The initial “survival phase” was shorter in western Canada due to greater mortality from trauma. Thereafter, survival plummeted in both series during the asphyxia phase, ending at 35 minutes burial, with mortality greater in Canada due to denser snow.
Deducing that victims unable to breathe had succumbed to asphyxia at the end of this 35 minutes, while those with a patent airway and an air space could survive longer until death from hypothermia at 90 minutes, the International Commission for Mountain Emergency Medicine (ICAR MEDCOM) published resuscitation recommendations and a management algorithm (Brugger et al., 2001).
However, this analysis did not consider actual clinical experience. The first systematic review of clinical evidence for these recommendations confirmed that duration of burial, airway patency, core temperature and serum potassium levels were reliable predictors of survival (Boyd et al., 2010) and, after expert review by the International Liaison Committee for Resuscitation (ILCOR), were included in the 2010 BLS and ALS2 Resuscitation Guidelines for North America and Europe (Soar et al., 2010; Vanden Hoek et al., 2010).
Although current adoption of these recommendations approximates 75%, there are substantial failures, notably in initiation or withholding of CPR and triage to extracorporeal circulation rewarming (heart-lung bypass) (ECR) (Brugger, 2011). Additionally, recent research in avalanche trauma (Hohlrieder et al., 2007; Boyd et al., 2009), survival analysis (Haegeli et al., 2011) and hypothermia management (Brown et al., 2012) has shifted emphasis.
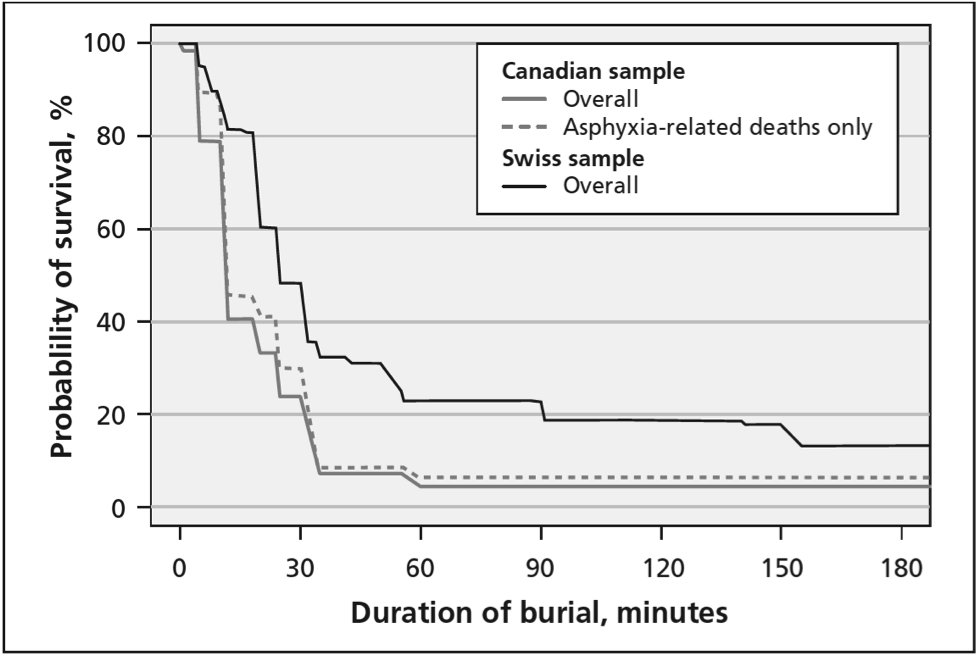
FIG. 1: OVERALL SURVIVAL CURVES FOR PEOPLE COMPLETELY BURIED IN AVALANCHES IN CANADA (N = 301) AND SWITZERLAND (N = 946) FROM OCT. 1, 1980, TO SEPT. 30, 2005, BY DURATION OF BURIAL (DUMBGEN COMPARISON: P = 0.001). THE DOTTED LINE REPRESENTS THE CANADIAN SURVIVAL CURVE INCLUDING ONLY ASPHYXIA-RELATED DEATHS (N = 255). EXTRACTED FROM HAEGELI ET AL., 2011.
METHODS
A structured clinical-literature review of the components of the 2001 algorithm was performed using an ILCOR worksheet format after establishing subject matter, objectives and inclusion/exclusion criteria a priori at a TOPIC meeting of the ICAR MEDCOM. This format examined each of 27 components using individual PICO (population, intervention, comparator, outcome) questions as well as 10 general questions. Findings were presented by the working group to a SCIENCE meeting of the ICAR MEDCOM for expert debate, and consensus recommendations were developed at a MANUSCRIPT meeting in October 2011.
RESULTS
Keyword- and hand-searching found 3,530 publication citations in the peer-reviewed clinical literature of which 96 articles were scrutinized in detail for content, study design and methodological quality. Thirty-seven recommendations were developed, classified for benefit and a simplified algorithm was developed. These recommendations and an algorithm (Fig. 2) for ALS personnel have been published (Brugger et al., 2012). Below is an abridged text oriented to both BLS and ALS rescuers.
GENERAL RECOMMENDATIONS
Safety and welfare
The safety and welfare of rescuers and all others remain paramount.
Companion and organized rescue
Prompt extrication with initiation of BLS resuscitation remains the priority for companions. Organized rescue is best mobilized early, ideally by helicopter, with rescue-trained emergency physicians or paramedics equipped with critical medical and safety kit, plus dogs with handlers.
Airway patency and air pocket
Rescuers are to dig from the side and, in burials longer than 35 minutes, note whether the airway is patent +/- an air pocket present.
General measures
To mitigate against the common rescue collapse from cardiac arrhythmias, hypothermic victims are best managed gently, with minimal truncal and limb movements, without rough motion or inappropriate chest compressions, and kept in a horizontal position.
Dry insulation includes insulation from the snow surface as well as from continued conductive, convective and radiant heat loss. Assemblies include blankets, padded rescue bags and outer windproof and waterproof reflective foils. Wet clothing may be replaced with dry layers if efficient although adding thick insulation over wet clothing is equally effective and usually more practical (Henriksson et al., 2012).
Field rewarming is principally prevention of further heat loss plus chemical heat packs, although more sophisticated rewarming with specific equipment may be indicated if evacuation is prolonged. Heated humidified inspiratory air or oxygen requires field-usable equipment and does not greatly reduce heat loss but may be indicated in prolonged transports.
Oxygen is indicated for any degree of asphyxia and will reduce the risk of arrhythmias in hypothermia (Danzl, 2012). Pulse oximetry may be unreliable with cold extremities and device malfunction from the cold, bright light and high altitude (Luks and Swenson, 2011).
Monitoring
Victims of significant involvement are best monitored throughout evacuation and ideally from the moment they are exposed. This includes electrocardiographic (ECG) monitoring with an AED or monitor-defibrillator. Core temperature is most reliably measured in the lower oesophagus in victims that have an endotracheal tube (tube in the trachea) in place. A medical thermistor probe is preferable although inexpensive probes from indoor/outdoor thermometers can be sufficiently accurate (Pasquier et al., 2012). Epitympanic (ear drum temperature) probes are accurate if used appropriately (Walpoth et al., 1994). Rectal temperatures provide a reasonable initial temperature (Danzl, 2012) although require undressing the victim and lag during rewarming. Other temperatures are likely unreliable. Clinical staging is unreliable if asphyxia or trauma impairs mentation.
Airway management and ventilation
An unresponsive victim without an advanced airway is best transported in the recovery position with the cervical spine stabilized as well as possible. Airway interventions have low risk of inducing arrhythmias and include oropharyngeal airways as well as advanced airways such as endotracheal intubation or supraglottic airways (such as the laryngeal tube). Advanced airways protect against aspiration of vomitus and allow better victim access and spinal stabilization with the victim supine.
Ventilation is indicated when breathing is inadequate and always with chest compressions in CPR.
Trauma management
Pneumothorax is managed with needle thoracostomy (large-bore needle through the chest wall) or open thoracostomy (hole through the chest wall), ideally in a victim that is ventilated with an advanced airway.
Severe limb bleeding is managed with tourniquets. Other trauma modalities additionally include splinting, wound care, analgesia and antibiotics for open fractures.
Trauma victims are best transported to the medical centre that is most appropriate for their injuries, directly to a dedicated trauma centre3 if severe.

MANAGEMENT SCENARIOS
Alert victim
These are normothermic or mildly hypothermic. After assessment add insulation with or without changing wet clothing and allow active movement that will likely be sufficient to rewarm them. They may ingest warm clear sugar-containing fluids that are not alcoholic or strongly caffeinated so long as they are not likely to require sedation or anaesthesia in less than two hours and not significantly injured. Oral fluids will maintain hydration, especially if evacuation is delayed or prolonged.
If the involvement was clearly not life-threatening, then a decision may be made for them to remain in the field. However, if the involvement was potentially life-threatening they are best evacuated to the nearest emergency department for advanced assessment and observation as delayed complications may occur.
Poorly responsive victim with vital signs
These are asphyxiated +/- moderately or severely hypothermic. They are to be closely monitored, ideally with ECG monitoring as early as possible due to the risk of rescue collapse and arrhythmia. Core temperature will be very useful especially for disposition decisions. All general measures and other management modalities become critical.
Transport to the nearest hospital for advanced assessment, intervention and observation is indicated. If significantly asphyxiated, this would best be a hospital with an ICU. Seriously injured victims are best transported directly to a trauma centre. Hypothermic victims need rewarming with modalities such as the forced-air rewarmers most commonly used in surgical programs. However, if there is evidence of cardiac instability, such as ventricular arrhythmias on the ECG, or if the core temperature is <28°C (less than 28°C) direct transport to a centre4 with advanced extracorporeal rewarming (ECR), such as cardiopulmonary bypass, is preferable due to the risk of cardiac arrest during rewarming.
Victim with no vital signs with burial duration less than 35 minutes
These are asphyxiated and only mildly hypothermic. If lethal trauma is found, such as unsurvivable decapitation or truncal transection, resuscitation is withheld. Otherwise, prompt exposure and extrication with BLS including ventilations, with AED/ECG monitoring and defibrillation if indicated/prompted, +/- ALS are started expediently.
If clinical improvement results from resuscitation or any cardiac rhythm is seen on ECG or an AED prompts defibrillation, then resuscitation should continue to the nearest hospital, ideally with an ICU. If no improvement is found after 20 minutes of resuscitation and only asystole (flat line) has been seen on ECG or an AED does not prompt defibrillation then resuscitation may be terminated in the field (Soar et al., 2010; Vanden Hoek et al., 2010; Paal et al., 2012).
Victim with no vital signs with burial duration more than 35 minutes
These have suffered cardiopulmonary arrest from prolonged asphyxia or hypothermia. If lethal trauma is found or the whole body is frozen, resuscitation is withheld.
If they have an obstructed airway they have arrested from prolonged asphyxia, which after 35 minutes has a very poor prognosis, and resuscitation may be withheld (Soar et al., 2010; Vanden Hoek et al., 2010).
If the airway is patent they may have arrested from prolonged asphyxia with the resultant poor prognosis; but alternatively they may have been able to breathe and the arrest may have been from significant hypothermia and the victim may therefore be salvageable. Therefore, if the core temperature is found >32°C they are principally asphyxiated and a resuscitation attempt may be initiated but terminated if no improvement is noted after 20 minutes and only asystole is seen on the ECG or an AED does not prompt defibrillation. But, if the core temperature is <32°C then arrest may be from hypothermia and resuscitation is continued and the victim is transported preferably to a centre with ECR5. If the duration is not known and understanding that a core temperature of <32°C can only occur after at least 35 minutes of cooling, a core temperature of <32°C may therefore be a surrogate for burial longer than 35 minutes (Boyd et al., 2010; Vanden Hoek et al., 2010).
CPR is not modified for hypothermic arrest victims although a longer check of 60 seconds for vital signs is indicated as pulses may be indistinct. Persistent breathing or movement should prompt “watchful waiting” but if no signs of life are found then CPR is best started and continued. Defibrillation is performed if prompted by AED or indicated by ECG although repetitive defibrillation (over three attempts) may not be successful due to the cold heart being very irritable. ALS medications have only been shown effective in animal studies so judicial use is appropriate (Brown et al., 2012). No intervention is to delay transport of hypothermic arrest victims. Note is made that successful rewarming has resulted in good survivals after prolonged CPR of up to six and a half hours (Brown et al., 2012).
If the duration of burial or the status of the airway is unknown or a prolonged transport to ECR is being considered, then a serum potassium level (K+) at an emergency department, best in the direction of the ECR centre, may assist. If the K+ is <8mmol/L then survival is possible vs. >12mmol/L which is not survivable (Boyd et al., 2010; Soar et al., 2010; Vanden Hoek et al., 2010; Brown et al., 2012). A K+ between 8 and 12mmol/L may assist in a decision made with consideration of all factors.

VICTIMS WITH NO VITAL SIGNS THAT ARE BURIED LONGER THAN 35 MINUTES BUT THAT HAVE A PATENT AIRWAY ARE LIKELY TO HAVE SUFFERED A CARDIAC ARREST FROM SEVERE HYPOTHERMIA AND ARE BEST TRANSPORTED TO EXTRACORPOREAL RE-WARMING WITH HEART-LUNG BYPASS. // INNSBRUCK MEDICAL UNIVERSITY ARCHIVES
TRIAGE
Where multiple victims exceed available resources then triaging becomes necessary, especially when other victims remain buried. Victims without vital signs, especially if in asystole, are far less likely to survive and place high demands on resources. Victims exhibiting major trauma that appears likely lethal are not likely to survive. Extremely hypothermic victims, especially if their core temperature is the same as ambient temperature and is less than 10°C, are unlikely to survive. A triage algorithm for avalanche incidents that incorporates avalanche and triage concepts has been published (Bogle et al., 2010).
CONCLUSION
Important field recommendations range from simple evidence-based victim-handling measures to integrating critical factors in crucial decisions that include prehospital termination of resuscitation. Advanced airway use as well as AED and core temperature monitoring are more relevant with improved training of avalanche professionals. Trauma management includes the use of tourniquets as well as decompression of pneumothorax. Triage of multiple victims on-site, and those severely hypothermic to appropriate centres, is enabled using the integrated avalanche resuscitation algorithm.
CONFLICT OF INTEREST
None of the authors have any financial conflict of interest. All authors have published on mountain medicine.
REFERENCES
Bogle, L.B., Boyd, J.J. and McLaughlin, K.A., 2010. Triaging multiple victims in an avalanche setting: the Avalanche Survival Optimizing Rescue Triage algorithmic approach. Wilderness Environ Med, 21(1): 28-34.
Boyd, J.J,, Brugger, H. and Shuster, M., 2010. Prognostic factors in avalanche resuscitation: a systematic review. Resuscitation, 81(6): 645-652.
Boyd, J.J., Haegeli, P., Abu-Laban, R.B., Shuster, M. and Butt, J.C., 2009. Patterns of death among avalanche fatalities: a 21-year review. CMAJ, 180(5): 507-512.
Brown, D.J., Brugger, H., Boyd, J.J and Paal, P., 2012. Accidental hypothermia. New England Journal of Medicine, 367(20): 1930- 1938.
Brugger, H., 2011. Avalanche accidents: ILCOR Guidelines 2010 & ICAR MEDCOM algorithm. Proceedings ICAR General Assembly, Are, Sweden.
Brugger, H., Durrer, B., Adler-Kastner, L., Falk,. M. and Tschirky F., 2001. Field management of avalanche victims. Resuscitation, 51(1): 7-15.
Brugger, H., Durrer, B. and Boyd, J.J., 2004. On Site Treatment of Avalanche Victims. Avalanche News, 71(Winter 2004-05): 30-33.
Brugger, H., Durrer, B., Elsensohn, F., Paal, P., Strapazzon, G., Winterberger, E., Zafren, K. and Boyd, J.J., 2012. Resuscitation of avalanche victims: Evidence-based guidelines of the international commission for mountain emergency medicine (ICAR MEDCOM): Intended for physicians and other advanced life support personnel. Resuscitation, 2012 Nov 2. pii: S0300- 9572(12)00876-3. doi: 10.1016/j.resuscitation.2012.10.020. [Epub ahead of print]
Brugger, H. and International Commission for Alpine Rescue, 2006. Time is Life - medical training in avalanche rescue. IKAR-CISA : Newport Music [distributor]
Danzl, D. F., 2012. Accidental Hypothermia. Wilderness medicine. Auerbach P. S.. Philadelphia, Mosby Elsevier: 116-142.
Falk, M., Brugger, H. and Adler-Kastner, L., 1994. Avalanche survival chances. Nature, 368(6466): 21.
Haegeli, P., Falk, M., Brugger, H., Etter HJ and Boyd J.J., 2011. Comparison of avalanche survival patterns in Canada and Switzerland. CMAJ, 183(7): 789-795.
Henriksson, O., Lundgren, P., Kuklane, K., Holmer, I., Naredi, P. and Bjornstig, U., 2012. Protection against Cold in Prehospital Care: Evaporative Heat Loss Reduction by Wet Clothing Removal or the Addition of a Vapor Barrier-A Thermal Manikin Study. Prehosp Disaster Med, 27(1): 53-58.
Hohlrieder, M., Brugger, H., Schubert, H.M., Pavlic, M., Ellerton, J. and Mair, P., 2007. Pattern and severity of injury in avalanche victims. High Alt Med Biol, 8(1): 56-61.
Luks, A. M. and Swenson, E.R., 2011. Pulse oximetry at high altitude. High Alt Med Biol, 12(2): 109-119.
Paal, P., Milani, M., Brown, D., Boyd, J.J. and Ellerton, J., 2012. Termination of Cardiopulmonary Resuscitation in Mountain Rescue. High Alt Med Biol, 13(3):200-8.
Pasquier, M., Rousson, V., Zen Ruffinen, G. and Hugli O., 2012. Homemade thermometry instruments in the field. Wilderness Environ Med, 23(1): 70-74.
Soar, J., Perkins, G. D., et al., 2010. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation, 81(10): 1400-1433.
Vanden Hoek, T. L., Morrison, L. J., et al., 2010. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 122(18 Suppl 3): S829-861.
Walpoth, B.H., Galdikas, J., Leupi, F., Muehlemann, W., Schlaepfer, P. and Althaus, U., 1994. Assessment of hypothermia with a new "tympanic" thermometer. J Clin Monit, 10(2): 91-96.
1) International Commission for Alpine Rescue
2) BLS = Basic Life Support; ALS = Advanced Life Support.
3) For example - Vancouver General Hospital, Royal Inland Hospital in Kamloops, Kelowna General Hospital or Foothills Medical Centre in Calgary.
4,5) For example - Vancouver General Hospital, Foothills Medical Centre in Calgary or University Hospital in Edmonton. Near future - Kelowna General Hospital